
[ad_1]
This is the first part of a major Financial Times series, Coronavirus: could the world have been spared?, investigating the global response to the crisis and whether the disaster could have been averted.
The FT has spoken to dozens of medical professionals, government officials and ordinary citizens in Wuhan to find out what really happened in the first weeks of the outbreak.
During the investigation, some of the people approached were threatened by police, who said that the FT had come to the city with “malicious intent”. Police harassment of virus victims, their relatives and anyone hoping to speak to them is continuing, raising doubts about whether Xi Jinping’s administration is really willing to facilitate the impartial investigation into the pandemic that it has promised the world.
EARLY WARNINGS
The virus arrives

It was in late December, while scrolling through his Twitter feed, that Gao Fei first noticed chatter about a possible virus outbreak in Wuhan.
Mr Gao, who had grown up near Wuhan, regularly used virtual private network software to hop over the “Great Firewall”, as China’s internet censorship regime is more popularly known, to access banned sites such as Twitter. While government officials and state media were saying very little about the virus, he was determined to learn more.
As doubts about the true size of the outbreak grew through January, Mr Gao, 33, decided to rush home from southern Guangdong province where he was working as a welder. He arrived in his home village, about 120km from Wuhan, on January 21, just a day after the Chinese government finally broke its silence about the epidemic and confirmed the virus was spreading human-to-human.
The Chinese government had formally notified the World Health Organization on January 3 that a “severe pneumonia of unknown etiology” — science speak for a mysterious new respiratory disease — had been discovered in Wuhan, capital of Hubei province with a population of 11m. But for the first three weeks of January, Chinese officials said there were only a few dozen confirmed cases and downplayed the risk of human transmission.

Aghast to find life in his village unchanged, Mr Gao confronted local officials. “They told me they hadn’t received any orders from higher level [officials], so there was nothing they could do,” he told the Financial Times. “People in my village were still visiting relatives and gathering as normal.”
On January 23, the same day that Wuhan was subjected to a strict quarantine, he ventured one rung higher up China’s administrative hierarchy, visiting the county government. The message there was the same: “They told me they needed to wait for orders from higher level municipal officials” in Huanggang, the city that encompasses Mr Gao’s village.
“It was shocking,” said Mr Gao. “By the time the situation in Wuhan was totally out of control, other cities just one hour’s drive away were totally unprepared . . . A lot of things could have been avoided if people had only been told the truth about the virus.”
BLAME GAME
China and the WHO’s united front

The sloth and complacency Mr Gao encountered in his home village is central to the ongoing geopolitical blame game over the coronavirus pandemic, which has now infected 39m people globally, killed more than 1m and devastated economies on a scale not seen since the Great Depression of the 1930s.
On January 14, a day after coronavirus was confirmed to have spread beyond China, from Wuhan to Bangkok, the country’s top health officials convened a confidential meeting in Beijing at which they fretted about a “high” risk of human-to-human transmission. The sudden appearance of Wuhan-linked cases in Bangkok and, a few days later, Tokyo suggested that Wuhan’s official case count, which stayed at only a few dozen through mid-January, was nonsense.
Coronavirus: could the world have been spared?

The coronavirus pandemic has killed more than 1m people across the globe. But could it have been averted? A unique FT investigation examines what went wrong — and right — as Covid-19 spread across the world
Part 1: China and Covid-19: What went wrong in Wuhan
October 18: The global crisis — in data
October 20: Why coronavirus exposed Europe’s weaknesses
October 21: Will coronavirus break the UK?
October 22: How New York’s mis-steps let Covid-19 overwhelm the US
October 23: What Africa taught us about coronavirus, and other lessons the world has learnt
In reaction to the news from Bangkok and Tokyo, epidemiologists at Imperial College London released a study estimating that for the virus to be spreading beyond Chinese borders, there had to be about 4,000 symptomatic people in Wuhan. Yet during this critical week a large annual legislative meeting went ahead and a now infamous pre-Chinese new year dinner, attended by 40,000 families, was held in the city on January 18.
The Chinese government and the WHO also downplayed growing concerns about whether the disease could be transmitted readily between humans. Speaking at a press conference in Geneva on January 14, Maria Van Kerkhove, acting head of the WHO’s emerging diseases unit, was quoted by Reuters as saying there had been “limited human-to-human transmission” in Wuhan.
The WHO scrambled to clarify Dr Van Kerkhove’s reported comments, saying she had only mentioned that human transmission was “possible” and “may” be occurring. “There was a misunderstanding at the press briefing,” the WHO told the FT that day. “Preliminary investigations conducted by the authorities have found no clear evidence of human-to-human transmission.” Another six days would pass before Zhong Nanshan, a Chinese epidemiologist and a government adviser, finally confirmed in an interview with state media on January 20 that the virus could actually spread between people.
This was the start of what would become a regular pattern during the initial stages of the pandemic. Externally at least, President Xi Jinping’s administration sought to downplay the potential threat of the virus and initially lobbied against “excessive actions”, such as the early declaration of a global health emergency and travel bans aimed at Chinese nationals.

Officially, it remains WHO policy not to support travel bans during pandemics — as the Chinese government urged in late January when its citizens were the primary targets of such bans. However by late March, when the virus was coming under control in China but spreading unchecked across Europe and the US, Beijing changed its mind about the wisdom of travel bans as it barred almost all foreign arrivals.
In a meeting with Mr Xi on January 28 in Beijing, Tedros Adhanom Ghebreyesus, WHO director-general, praised “the seriousness with which China is taking this outbreak, especially the commitment from top leadership and the transparency they have demonstrated, including sharing data and genetic sequence of the virus . . . WHO will keep working side-by-side with China and all other countries to protect health and keep people safe”.
Ross Upshur, a public health expert at the University of Toronto and a WHO consultant, notes that China has always had a lot of political sway at the WHO, and this has only increased since US president Donald Trump announced in April that he would withhold funding for the organisation. “It’s like David and Goliath, you’ve got big China and you’ve got Tedros . . . there’s an asymmetry of power there.”
China’s critics who blame Mr Xi and the Chinese Communist party for the ongoing catastrophe — including Mr Trump — contend that at the very least, his administration missed opportunities in late December and early January to slow the spread of the virus within China and around the world. Many argue this failure was a direct result of the ever more authoritarian tendencies and increasing opacity of China’s unique “party state” governance model.
“The coronavirus has alerted [the world] that China has become a threat to people’s livelihoods, and even their lives, around the world,” said Jimmy Lai, the Hong Kong pro-democracy print mogul and one of the party’s harshest critics. “Without freedom, the people of China are deprived of information and facts [they need] to take care of themselves.”
Grieving relatives: anger over human cost of cover-up

“The government cover-up cost my son his life,” said Zhong Hanneng, whose 39-year-old son, Peng Yi, died from Covid-19. “The government kept saying there was no human-to-human transmission and we believed them. We had a large family dinner on January 20 with 20 people.”
After Peng, a Wuhan primary school teacher with a young daughter, developed a fever, a CT scan of his lungs suggested he had contracted the virus. But the first hospital in the city where he sought treatment did not have enough test kits to confirm his condition and refused to admit him.
“Over the next two weeks we visited numerous hospitals,” said Ms Zhong. “They were all full.” When the family finally found one on Wuhan’s outskirts, no ambulance was available. Peng was transferred in the back of a small truck at about 1.30am on February 7. The bumpy 90-minute ride would be his last. He died in hospital 12 days later. “Before the virus my son had just paid off his mortgage and life couldn’t have been happier,” said Ms Zhong. “Now every day is a misery.”
Zhang Hai, a Wuhan native now living in the southern city of Shenzhen, also blames the government for a loved one’s death. In January he unwittingly arranged for his father, Zhang Lifa, to return to Wuhan for leg surgery. While in hospital his father contracted the virus and died a week later.
“The government knew how bad the virus was at an early stage but didn’t give a public warning and chose to cover up the truth. That has cost so many lives,” said Mr Zhang. He is now trying to sue the Wuhan government for Rmb2m ($294,000) in compensation, but China’s party-controlled courts will not take his lawsuit. Such citizen-suits alleging local government negligence after disasters are not uncommon in China, although they rarely succeed.
The Chinese government has defended its decision not to acknowledge publicly the seriousness of the outbreak, and the risk of human-to-human transmission, until January 20, arguing it was grappling with an incredibly complex situation in unclear circumstances. Dale Fisher, an infectious diseases specialist at Singapore’s National University Hospital, is sympathetic to this argument. “You’ve got to remember this was a novel virus and chaos is really normal, especially at the beginning of an outbreak,” said Dr Fisher, who has experience working in west African Ebola hotspots and was a member of a WHO delegation that visited China in mid-February. “You don’t want to push [the panic] button until you’ve got reasonable confidence [in your diagnosis].”
BATTLE STATIONS
A mounting catastrophe

As Wang Linfa toured Wuhan in mid-January, he had no inkling that he was witnessing the beginning of a global catastrophe.
Prof Wang is one of the world’s leading authorities on bat-borne diseases, but his presence in Wuhan at the early stages of the outbreak was a coincidence. A Shanghai native living in Singapore, where he is director of the emerging infectious diseases programme at Duke-NUS Medical School, Prof Wang travelled regularly to China to meet colleagues. His trip had been scheduled since early December.
Many of the initial cases in Wuhan had already been linked to a live wet market, a fact that triggered memories of the Sars epidemic that emerged in the winter of 2002-2003. Sars emanated from southern Guangdong province and Hong Kong, infecting more than 8,000 people and killing 774. The scientific consensus is that Sars originated in bats before transmitting to humans via an “intermediate host”, most likely a civet cat sold for food in a market.
“The news of the market was certainly a déjà vu moment,” said Prof Wang. “I was thinking to myself, ‘Oh my God’ it’s winter, just before Chinese new year, and the market . . . I really thought it must be similar to Sars.”
Prof Wang’s extensive experience working with Chinese medical institutions seemed reassuring as he toured Wuhan on January 15, 16 and 17. “Conditions [in China] are much, much better than 17 years ago,” he said. “Chinese doctors and scientists are first-class, among the leading scientists in the world. So I thought that even if this is like Sars, the impact will be smaller than Sars.”
Arriving in Wuhan by high-speed rail on January 14, Prof Wang noticed very few people wearing masks. There were also no temperature checks, both signs that would have suggested local and central government authorities were on high-alert. When he was entertained by his Chinese hosts as on many previous trips, “every meal we went to a public restaurant, [all] very crowded with people”. Only in the early morning hours of January 18 did he begin to fear the situation in Wuhan might be far more serious than he had realised.
As Prof Wang prepared to board his flight back to Singapore, he saw the authorities at battle stations. “They were doing very stringent temperature screening” before boarding, he said. “There were lots of cameras and security people and medical staff wearing full PPE. [If you had a] fever you were banned from travelling out of Wuhan.”
For the first time he felt afraid and moderated his behaviour: “I thought, it’s like a war zone, now it’s really serious.” He avoided contact with other passengers as best he could. The precautions he took may well have prevented him from contracting the virus, or worse. A woman on the same flight would later be confirmed as one of Singapore’s first coronavirus patients.

Prof Wang called China’s political system a “double-edged sword” that inhibited the country’s initial reaction to the outbreak, but eventually helped it to enforce effective containment measures. “It is not very effective in the early part of any outbreak because you’re not allowed to talk until the government says ‘OK, I’m convinced you’re right, you can talk’,” he said. “If China’s system becomes more democratic, it would help [with transparency] but it may make [containment] less effective.”
So far Chinese health officials have traced the first confirmed coronavirus case back to December 1, but the hunt for the pandemic’s true “patient zero” is likely to be futile. While the majority of people who contract the virus exhibit either mild symptoms or none at all, they can still spread it to others. In medical parlance, Covid-19 is caused by an “early shedding” coronavirus that spreads rapidly through communities because most people are not aware that they are infectious. Sars was a “late shedding” coronavirus — patients generally became infectious after they had been hospitalised, making it much easier to contain. “Hospital control we can easily implement to shut down things,” said Dr Fisher. “Community infection control is much more challenging.”
In this respect, finding the original coronavirus patient — the man, woman or child who ate the bat-bitten cat, pangolin or other as yet undetermined intermediate host — is as difficult as finding the first person to contract a seasonal flu. “Patient Zero could be someone who spread to another 30 patients but never knew he was infected,” said Prof Wang.
confusion and denial
Inside Wuhan Central Hospital

Three weeks before Mr Xi’s administration publicly acknowledged that a deadly new respiratory disease was spreading through one of China’s largest cities, doctors at Wuhan Central Hospital realised they had a problem.
On December 29 at 2pm, Yin Wei, a doctor in the hospital’s public health department, received a call from a colleague reporting that four patients were displaying symptoms of viral pneumonia. All four patients, Dr Yin’s colleague added, had come from a local seafood market.
According to an internal report later prepared by Dr Yin and viewed by the FT, he immediately notified the responsible health official in the local district government, Wang Wenyong. Mr Wang was not surprised by Dr Yin’s call.
“Wang replied that he had received similar reports from other hospitals and the Wuhan Center for Disease Control and Prevention couldn’t determine the cause of the disease after conducting multiple tests,” Dr Yin wrote. “Wang added that he would reply to me after reporting our hospital’s situation to his supervisor.”
At 4pm, three more cases of viral pneumonia were discovered at Wuhan Central Hospital. At 8pm, district CDC officials came to the hospital to collect patient samples, after which they told Dr Yin and his colleagues to wait.
Two days later, on December 31, they were still waiting. So Dr Yin called one of Mr Wang’s bosses at the district CDC to inquire about the test results. “I was told to wait for further notice,” Dr Yin wrote.
On January 3, Dr Yin tried again, asking Mr Wang if Wuhan Central should at least fill out an infectious disease report card (IDRC), an online reporting system shared by local and national healthcare authorities. Again, he was rebuffed. “Wang replied that we should wait for further notice from higher authorities before reporting a special infectious disease like this,” Dr Yin recalled in his report.
It was not until January 4, seven days after Dr Yin and his colleagues tried to alert city officials, that they were finally allowed to fill out IDRCs for all suspected cases of unknown viral pneumonia.
Mr Wang, the official repeatedly mentioned by Dr Yin, said that “Wuhan Central Hospital was looking to shift blame to me in the report”.
“I didn’t do anything wrong,” he told the FT, adding that everyone in the system was simply following orders. “Wuhan Central didn’t follow standards established by the city and provincial health commissions . . . [Yes] we were cautious in reporting cases early on. But that was a collective decision, not my own.”
Wuhan Central referred the FT’s requests for interviews with its administrators and doctors to the municipal government, which did not reply.
As medical staff at Wuhan Central tried to figure out what they were and were not allowed to report higher up the chain, central government officials from Beijing were already at ground zero in Wuhan. A delegation from the Chinese Center for Disease Control and Prevention first arrived on December 31, according to an official Chinese government chronology of its virus control efforts.
One academic who advises central government health officials said they even discussed in the first few days of the new year whether daily public briefings should be held. But Beijing officials did not do so until January 22, in part because of the chaotic situation in Wuhan. “The information [from Wuhan] was not clear,” said the adviser, who asked not to be identified. “There were lots of rumours and local officials’ attitude was say little or, if possible, say nothing. It was a mess.”
The WHO said that it asked Chinese government officials about the Wuhan outbreak on January 1 and received Beijing’s reply two days later, on January 3. Communist party officials have also acknowledged that Mr Xi gave orders concerning the evolving situation in Wuhan at a January 7 meeting of the politburo’s most senior body, the seven-man Politburo Standing Committee. According to a leading party journal, the president instructed officials to find the origin of the virus and “confirm the transmission mechanism as soon as possible”.
Another person who advises the State Council on public health matters said the problem ran deeper than the fog-of-war conditions on the ground in Wuhan. “The Chinese government, especially at local levels, lacks the ability to effectively communicate with the public in crisis situations,” he told the FT, also on condition of anonymity. “The main job of publicity departments is to keep the Communist party in power, not to promote transparency. The pandemic exposed the system’s weaknesses.”
The confusion among doctors at Wuhan Central about what information they were supposed to report to which authorities grew steadily over the first two weeks of January. They were variously advised by municipal and provincial health officials to “exercise caution” and “be cautious” before reporting any new cases, according to Dr Yin’s report.
On January 13, contradictory instructions from Wuhan’s health department and the municipal CDC finally caused Dr Yin’s temper to boil over. “Dear Director Wang,” he wrote. “We have a situation about reporting suspected cases. The health department said we should ask the CDC to collect samples and conduct investigations, but the CDC said they need to wait for instructions from the health department. This has prevented a suspected patient from being tested and investigated. We have no idea what has gone wrong. Can you help us figure out the problem?”
Within days, however, the patients falling through the cracks in the reporting system were the least of Wuhan Central’s problems. The hospital’s own staff were beginning to fall sick, with at least 56 hospitalised by January 24. An outbreak among hospital staff is a tragic but tell-tale sign that a disease is transmissible between humans.

Among the Wuhan Central doctors who lay dying in their own wards was Li Wenliang, a 33-year-old ophthalmologist and one of several medical staff reprimanded by police on January 3 for allegedly “spreading rumours” about the then mystery virus, although all they had done was discuss it among themselves in a private chat group. Li’s death in early February would provoke a firestorm of public anger, although one that was largely directed at the local government rather than the central government in Beijing.
With confusion rife across China through most of January, one of the biggest mysteries about the initial stages of the pandemic is why Wuhan-sized clusters did not emerge all over the country. According to Chinese flight data cited by state media, between December 30 and January 22 more than 465,000 people flew from Wuhan to 10 popular domestic destinations, from Beijing in the north to the southern resort city of Sanya. At the same time, far smaller flows of people from Wuhan to international destinations seeded the global cataclysm that is still unfolding.
The answer lies in the vastly different responses by governments in China and the Asia Pacific region, Europe and the US.
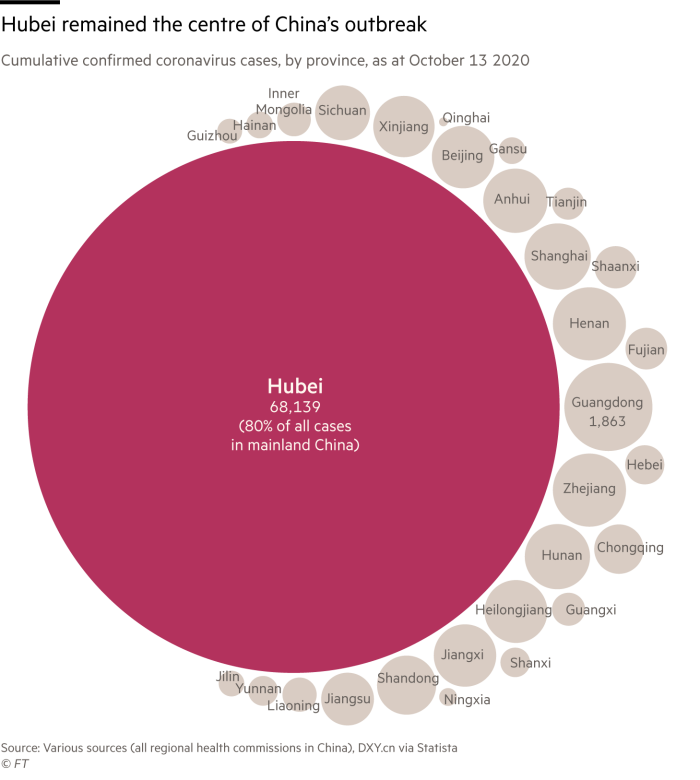
Real Chinese infection numbers were significantly higher than officially reported, but not recorded because almost the entire population was forced into strict lockdowns from late January through mid-February.
“Every province in China got infected within a month [of the Wuhan outbreak] and [their official case counts] generally settled into triple figures because their lockdowns were harsh,” said Dr Fisher. “Diagnoses weren’t made because everyone was staying at home. People with mild cases probably spread it to a couple of people in their family who also had mild cases and the virus just burnt itself out . . . Within three to four weeks they were able to unlock things.
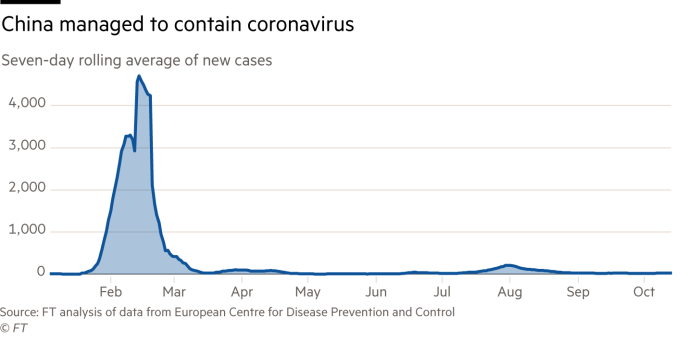
“I was in China [in mid-February] and was able to see the extent of the response,” he added. “Unbelievable lockdowns with trains not moving, aeroplanes all with covers on their engines, and absolutely clear blue skies in [often polluted] Beijing. So it did spread across China, but they just shut it down.”
Meanwhile other countries and territories in east Asia — most notably South Korea, Taiwan, Hong Kong and Singapore — used a more flexible mix of visitor bans, contact tracing and lockdowns milder than China’s to contain community spread of the virus effectively.
But for those countries that were quick to issue travel bans while doing little else in a co-ordinated, nationwide fashion, such as the US, it was too late.

Dr Fisher was speaking to the FT by phone from Singapore on the morning of August 28. As he did so, he was also watching a live TV feed of the final night of the US Republican National Convention. While responding to the FT’s questions, he occasionally interjected his amazement at the scene in Washington. “There’s Donald Trump’s daughter addressing everyone and she’s not wearing a mask!” he exclaimed at one point. “Nor is anyone else. They haven’t even distanced the seats!”
Dr Fisher’s view was that “another couple of weeks” of advance notice about the pandemic would not have helped many countries. He pointed out that despite it being confirmed that the virus could be transmitted from person to person on January 20, “it’s not like [everyone] jumped up and sprang into action”.
“Most of Asia really respected this, had systems ready to go, and did a lot of work in January and February for the day that was coming when they were going to get smashed,” said Dr Fisher. “Unfortunately, most of the rest of the world needed to get smashed to have that realisation. As we said in our February [WHO China delegation] report, this virus can have devastating health, social and economic effects but the world is not ready, in capacity or in mindset, to deal with it.”
Prof Wang added that for all of the Chinese system’s shortcomings in the earliest days and weeks of the outbreak, the rest of the world should have been on high alert. As soon as human-to-human transmission was confirmed and Wuhan went into quarantine a few days later, countries could have prepared themselves for its arrival as effectively as Taiwan and South Korea did, among others.
Most did not. In particular the Trump administration’s response will go down as one of the worst national security failures in the history of the US republic, with the virus breaching even the White House and the president himself. As Prof Wang said: “For other countries not to have taken [the virus] seriously, there’s just no excuse.”
Additional reporting by Qianer Liu and Anna Gross
[ad_2]
Source link